Eran Linder-Ganz (1), Noga Shabshin (2), Yacov Itzchak (2), Itzhak Siev-Ner (3), Amit Gefen (1)
(1) Dept. of Biomedical Engineering, Faculty of Engineering, Tel Aviv University, Tel Aviv, ISRAEL
(2) Dept. of Diagnostic Imaging, Chaim Sheba Medical Center, Tel Hashomer, ISRAEL
(3) Dept. of Orthopedic Rehabilitation, Chaim Chaim Sheba Medical Center, Tel Hashomer, ISRAEL
INTRODUCTION
Deep tissue injury (DTI) is a severe type of pressure ulcers affecting the viability of muscle tissue under bony prominences first [1]. Most researchers agree that prolonged elevated muscle tissue strains and stresses cause the onset of DTI. We recently showed that internal strain and stress distributions in muscle tissue of individuals can be evaluated by integrating Open-MRI examinations with subjectspecific finite element (FE) analyses [2]. However, sub-dermal soft tissue strain and stress data from paraplegic wheelchair users are missing in the literature. Our present goals were therefore (i) to determine the strain and stress distributions in the gluteus muscles and enveloping fat under the ischial tuberosities (IT) of paraplegic wheelchair users during sitting and lying in an Open-MRI, (ii) to compare the paraplegic data to those obtained previously from normal subjects [2], and (iii) to compare between results obtained from paraplegics in the sitting and lying postures, in order to quantify the effect of posture on sub-dermal tissue mechanical conditions, particularly intramuscular shear stress.
METHODS
The pilot studies reported herein were conducted with three paraplegic volunteers who depend on a wheelchair for the last 17-35 years (2 males, 1 females; age: 36-53 years, bodyweight: 70-80 kg). All studies were approved by the Helsinki committee of Sheba Medical Center, Israel (approval: #4045/2006) and informed consent was obtained from each participant. Imaging of the buttocks during sitting was performed in an open configuration MR system as described in [2]. The unique configuration of the open MR system allowed successful imaging of the buttocks during non-weight-bearing as well as weight-bearing sitting. Each patient was asked to sit comfortably, inside the MR field: first, on a rubber tire placed on the sitting surface of the system (non-weight-bearing sitting) and second, directly on the sitting surface (weight-bearing sitting). In addition, MR scans during prone (non-weight-bearing lying) and supine (weightbearing lying) postures were conducted for each patient. Interface pressures under the buttocks were also measured for all weight-bearing postures using a pressure mat (“Tactilus”, SPI Co.), in order to validate the patient-specific FE modeling by means of paired t-test comparisons of interface pressure measurements and respective computational (FE) predictions. The method of MR image processing and corresponding FE analyses of the images are described in detail in [2]. Briefly, for each MRI acquisition phase, the ITs with their surrounding soft tissues were scanned and two-dimensional (2D) coronal images were produced. Next, a three-dimensional (3D) FE model of the non-weight-bearing buttock geometry was produced from the non-weight-bearing MRI for each patient (FE models represented a slice through the buttocks with thickness of 4mm, corresponding to the MR image slice thickness). Each patient-specific model included bones, muscles, fat and skin (tissue constitutive laws were reported in [2]). Vertical sagging of the ITs toward the sitting surface in a weight-bearing posture was digitally measured in each patient by comparing the non-weight-bearing and weight-bearing MR images. We used bone sagging measurements as displacement boundary conditions for the patient-specific FE models. Additionally, external nodes that were in contact with the sitting surface were constrained for motion in the vertical direction. After solving the FE model for these boundary conditions, we compared the contours of the deformed gluteus muscles and enveloping fat, separately for each patient, with the corresponding contours seen in the weight-bearing MR image using the least-square method. By adjusting fat elastic moduli within a ±10% range, we were able to improve the fit of the FE solution to the MR image of actual tissue deformation. After obtaining this best possible fit (R2>0.9, p< 0.05), the FE solutions provided the local strain and stress tensors in the gluteus muscles and underlying fat for each patient.
Strain and stress distributions among wheelchair-users were compared to those found in normals during sitting in the same MRI setup using unpaired two-tailed t-tests, separately for each strain or stress component (that is, principal compression and tension, shear and von Mises). We also used paired two-tailed t-tests in order to compare strains and stresses found in sitting posture with those found in lying posture of each paraplegic patient. Throughout all the statistical tests, a p value below 0.05 was considered significant.
RESULTS
Peak interface pressures calculated from the patient-specific FE models overlapped with experimental data and were statistically indistinguishable similar per patient (p< 0.05), as evident from paired ttests ran separately for the left and right body sides. This was considered an indication that the models were all valid and that they adequately represented the mechanics of sitting and lying.
Using the integrated MRI-FE approach described above we were able to calculate the distributions of strains and stresses in muscle and fat under the ITs during sitting and lying. Figures 1 and 2 demonstrate the distributions of muscle and fat strains and stresses, respectively, in subject #4, a healthy female (age: 29 years, bodyweight: 55 kg), and patient #1, a paraplegic wheelchair-user (age: 43 years, bodyweight: 80 kg). On average, peak principal compression strain in the gluteus during sitting was 1.2-fold higher (p< 0.05) in the paraplegic patients (89±1%) than in the control group (74±7%, Figure 1). Likewise, peak principal compression stress in the gluteus during sitting was 3.2-fold higher (p< 0.05) for the wheelchair users (101±38 kPa) with respect to the normals (32±9 kPa, Figure 2a,b,3). Strain and stress peaks were located in the gluteus muscle, under the ITs in both groups. Figure 2c shows the principal compression stress distribution during lying, in the same patient (#1). For this specific patient it was found that maximal compression strain (89%), maximal compression stress (101 kPa) and maximal shear stress (62 kPa) during sitting are 1.6-fold, 3.7-fold and 4.1-fold higher than during lying (55%, 27 kPa and 15 kPa), respectively.
DISCUSSION
In this study we quantitatively demonstrated that permanent wheelchair-users develop significantly higher gluteus muscle strains and stresses during sitting compared with healthy controls, which explains why paraplegics are inherently more vulnerable to DTI. The dom
inant clinical approach for minimizing pressure ulcers nowadays is to relief pressures under bony prominences by training patients to change their posture frequently. Specifically, Griffith [3] recommended patients to lie down for 15 minutes following every 2 hours of sitting. The present study supports these recommendations as maximal gluteal stresses (compression and shear) in the buttocks of paraplegics decreased by ~75% in the lying posture compared with sitting. Although a larger-scale study is needed, the present results are the first ones in the literature to quantify internal gluteal strains and stresses during sitting and lying in paraplegic subjects, by means of an objective standardized engineering analysis. Data acquisition from additional paraplegic subjects is underway in our research group to strengthen the statistical power of our studies.
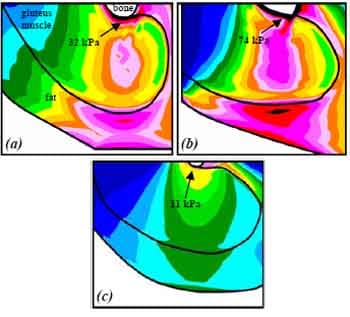
Figure 1. Principal compression strain distributions in the right gluteus of healthy (a) and paraplegic (b) subjects.
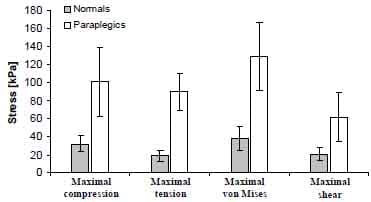
Figure 2. Principal compression stress distributions in the right gluteus of seated healthy (a), seated paraplegic (b) and (c) lying paraplegic subjects.
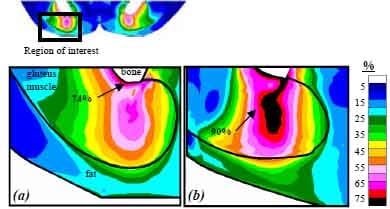
Figure 3. Peak gluteal stress values in normals versus paraplegics during sitting. All stress component values are significantly different between the paraplegic and control groups (p<0.05).
REFERENCES
- Black, J. M., National Pressure Ulcer Advisory Panel., 2005, “Moving toward consensus on deep tissue injury and pressure ulcer
- Linder-Ganz, E., Shabshin, N., Itzchak, Y., and Gefen, A., 2006, “Assessment of mechanical conditions in sub-dermal tissues during sitting: A combined experimental-MRI and finite element approach,” J Biomech, in press. PMID 16920122.
- Griffith, B. H., 1963, “Advances in the treatment of decubitus ulcers,” Surg Clin North Am, 43, pp. 245-260.


