G. 0. Gey, T. Rudd, and R. A. Bruce
From University of Washington and Affiliated Hospitals, Seattle, Washington, U.S.A.
The case is reported ofa 63-year-old white man with mild angina pectoris, whose systolic pressurefell 30 mmHg (4 0 kPa) with maximal exercise, without chest pain but with accompanying dizziness. Grafting the internal manmmary arteries into the mid left anterior descending and obtuse marginal arteries improved regional myocardial perfusion and increased maximal cardiac output 24 per cent and maximal systolic pressure 32 per cent.
Myocardial revascularization for ischaemic heart disease is the most common heart operation in the United States. Primarily, it is considered an operation for the treatment of angina pectoris. Reports of myocardial function before and after revascularization, however, have shown little increase in cardiac output with maximal exercise testing and a decrease in stroke volume at all levels of exercise (McDonough, Danielson, and Foster, 1974).
Case report
This case report describes a 63-year-old white man with a two-year history of mild angina pectoris who had evidence of myocardial ischaemia with exercise, a profound fall in blood pressure with exercise (Thomson and Kelemen, 1975), and accompanying symptoms of light-headedness (Irving and Kitchin, 1975), but no chest pain. On advice from his personal physician, he participated in a jogging programme, but without improvement, and was referred to the University of Washington Division of Cardiology for evaluation. His past medical history was interesting in that he had had varicose veins removed (greater saphenous) several years before his present symptoms and his family history was positive for heart attack and stroke.
On physical examination, his blood pressure was 130/86 mmHg (17-3/11*4 kPa) and his heart rate 72 beats/min. He was in no acute distress. His neck veins were flat at 45 degrees elevation, and his chest was clear to percussion and auscultation. His heart rhythm was regular and he had physiological splitting and an S4 gallop. Peripheral pulses were normal and equal. There was no evidence of hepatic enlargement. His legs had the scars from surgical removal of the greater saphenous veins and superficial varicosities of the lesser.
The 12-lead resting electrocardiogram was within normal limits. Chest x-ray showed a normal heart size; lung fields were clear.
Maximal exercise testing using the Bruce multistage protocol lasted 431 seconds (71 seconds into stage III). Blood pressure at rest was 115/70 mmHg (15-3/9-3 kPa), heart rate 65 beats/min. At maximum effort, blood pressure was 85/40 mmHg (11.3/5.3 kPa), heart rate 145 beats/min. The patient stopped with dizziness and dyspnoea. He had no chest pain. Auscultation revealed a pronounced S4 gallop. The electrocardiograph bipolar CB5 lead recorded a distinct ST segment depression of 4 mm, persisting for seven minutes.
Angiographic studies showed a 100 per cent occlusion of the proximal left anterior descending coronary artery, with retrograde filling from the right coronary artery which had multiple lesions of less than 50 per cent. There was also a tight 85 per cent stenosis proximal to the obtuse marginal artery. Left ventricular contraction was good and symmetrical. Left ventricular end-diastolic pressure was 9 mmHg (1*2 kPa) before left ventricular angiography and 12 mmHg (1*6 kPa) after injection of 50 ml contrast medium.
Because of the unusual symptoms and fall in blood pressure with exertion, the patient was evaluated with further exercise studies after giving his informed consent. A Swan-Ganz catheter was placed in the pulmonary artery and an arterial catheter in the brachial artery (Seldinger technique) under local xylocaine anaesthesia. Pressure measurement and cardiac output (Fick method) were determined at rest, each stage of exercise, and during the early recovery period. The results are shown in Table 1. During the exercise test with catheters inserted, the patient was able to achieve 97 5 per cent of maximum oxygen uptake (V02 max) measured by the first exercise test (without catheters). Maximum cardiac output (Qmax) was reached during stage II (12.45 litres/min), as was maximum stroke volume (SV max) (113 ml). Thereafter () and SV both fell, accompanied by a fall in mean systemic pressure to 75 mmHg (10 0 kPa) and a compensatory increase in AV 02 difference. Because of his varicose veins, the exercise test was repeated after leg-wrapping to establish whether the fall in blood pressure could be explained by the abnormal venous capacitance of the remaining varicose veins. The results are shown in Table 1, and represent no appreciable improvement.
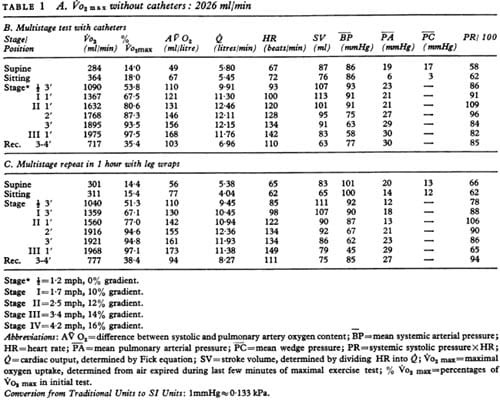
TABLE 1 A. Vo2 max without catheters: 2026 ml/min
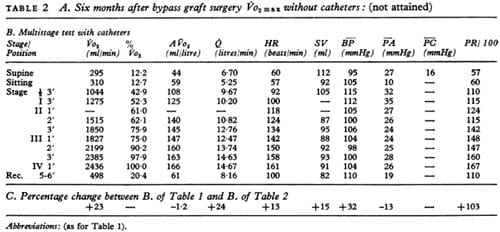
TABLE 2 A. Six months after bypass graft surgery Vo2 max without catheters: (not attained)
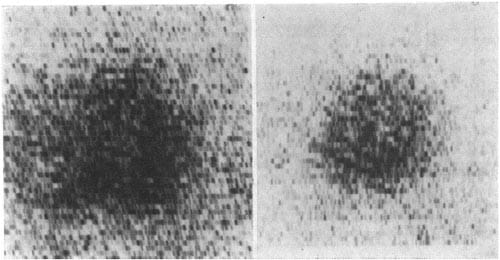
FIG. 1 – Left anterior oblique views of the myocardial 81Rh perfusion image recorded during independent exercise tests. Duration was identical, but the preoperative image was recorded at maximal exertion, and therefore the postoperative image was submaximal.
Two months later the patient had a bypass operation, grafting the internal mammary arteries to the mid left anterior descending (flow rate 55 ml/min) and obtuse marginal arteries (flow rate 25 ml/min). At operation, calcific atherosclerosis was noted in his distal right coronary and left main coronary arteries. The bypass surgery took 139 minutes and the operative procedure and postoperative period in hospital were without complications.
Six months after the operation, the patient volunteered for restudy. The results are shown in Table 2. There was a pronounced improvement in duration of the exercise test, which continued through one minute of stage IV. Maximum cardiac output was now 14-6 litres/min and stroke volume slightly lower (105 ml) than on the previous occasion. During exercise, the mean systolic pressure fell by only 10 mmHg (1.3 kPa), a distinct change from the previous tests. The patient no longer complained of light-headedness. Myocardial perfusion scanning using 8″Rh before and after operation showed an obvious improvement in the perfusion of the region of the left anterior descending artery. The standardized exercise tests were of the same duration.
Discussion
This case illustrates an unusual finding, in that the fall in systemic pressure with exercise accompanied the patie
nt’s complaint of light-headedness because cardiac output was limited by ischaemic heart disease. Resting angiographic studies showed normal left ventricular function, as did the myocardial perfusion scans done at rest. Myocardial revascularization brought about a definite improvement in maximal cardiac output and maximal systolic pressure, an uncommon occurrence with this procedure (Fig. 2). It suggests reversible exertional left ventricular dyskinesis. This case illustrates the benefit of adequate study with a maximal exercise testing procedure in the evaluation of ischaemic heart disease.
The authors wish to acknowledge the assistance of Dr. J. L. Petersen and Dr. L. R. Sauvage in the medical and surgical aspects of management of this patient.
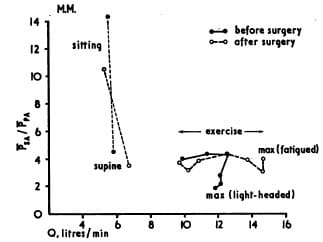
FIG. 2 Ratio of mean systemic pressure over mean pulmonary pressure to cardiac output at rest, supine and sitting, and then at each stage of exercise. Evidence of left ventricular failure preoperatively is noted at the second minute of stage II and in the progressive fall thereafter. Postoperatively, the pressure ratio remains fairly consistent, with the continued rise in cardiac output.
References
- Irving, J. B., and Kitchin, A. H. (1975). Syncopal attacks as symptom of severe coronary artery disease. British Medical Journal, 1, 555.
- McDonough, J. R., Danielson, R. A., and Foster, R. K. (1974). Maximal cardiac output before and after coronary artery surgery in patients with angina. American Journal of Cardiology, 33, 154.
- Thomson, P. D., and Kelemen, M. H. (1975). Hypotension accompanying the onset of exertional angina. Circulation, 52, 28.


