Paul E. Kobza, MD, Jeffrey E. Budoff, MD, Ming-Long Yeh, PhD, Zong-Ping Luo, PhD, Houston, TX
Purpose: To examine the effects of scaphoid retention, inclusion, and excision on wrist motion and radiolunate contact characteristics in a cadaveric model after simulated 4-corner fusion with rigid internal fixation.
Methods: Seven fresh-frozen cadaveric upper extremities were examined. For all surgical manipulations the motion was measured and contact characteristics were assessed using ultra-low prescale pressure-sensitive film.
Results: Compared with the intact specimen, simple 4-corner fusion with scaphoid retention led to a significant decrease in extension, radial deviation, and ulnar deviation, but no change in radiolunate contact characteristics. After 4-corner fusion there was no significant difference in motion or radiolunate contact characteristics between scaphoid retention and scaphoid inclusion. After 4-corner fusion scaphoid excision allowed significantly greater radial deviation compared with scaphoid retention and scaphoid inclusion. Compared with the intact specimen 4-corner fusion with scaphoid excision also led to a significant increase in radiolunate contact area and mean contact pressure.
Conclusions: When performing 4-corner arthrodesis in the absence of radioscaphoid arthritis, scaphoid excision may improve motion at the cost of increased mean radiolunate contact pressure. (J Hand Surg 2003;28A:904–909. Copyright © 2003 by the American Society for Surgery of the Hand.)
Key words: Midcarpal fusion, partial wrist arthrodesis.
Introduction
Four-corner partial wrist arthrodesis (lunate, triquetrum, capitate, and hamate) is a relatively common wrist reconstruction and often is used in the treatment of the scaphoid lunate advanced collapse pattern of arthritis.1–3 This pattern of arthritis includes degeneration of the radioscaphoid articulation, necessitating scaphoid excision.
Although previous studies have examined motion and joint contact characteristics after various partial intracarpal arthrodeses,4–6 a review of the literature was almost silent on the optimum management of the scaphoid when performing a 4-corner limited wrist arthrodesis for indications that do not involve radioscaphoid arthritis such as midcarpal instability, isolated midcarpal arthritis, or lunotriquetral dissociation with a fixed volar intercalated segmental instability alignment of the lunate. When performing 4-corner arthrodesis in cases without radioscaphoid arthritis, Taleisnik7 favors scaphoid inclusion and Weiss et al8 prefer scaphoid retention, but neither explains the rationale for their preference.
This article examines the effects of scaphoid retention, inclusion, and excision on wrist range of motion, and radiolunate contact characteristics after 4-corner arthrodesis in a cadaveric model using rigid internal fixation. The null hypothesis was that there was no significant difference in motion or contact characteristics between the intact specimen, 4-corner arthrodesis with scaphoid retention, 4-corner arthrodesis with scaphoid inclusion, and 4-corner arthrodesis with scaphoid excision.
Materials and Methods
Nine fresh-frozen cadaveric upper extremities were examined visually and radiographically to ensure that no intracarpal ligament injury, carpal malalignment, or other pathology affecting the wrist or forearm existed. The radius was sectioned at the midforearm level, and the ulna was sectioned 7 cm proximal to the distal radioulnar joint to allow the radius to be rotated while clamped. The superficial soft tissues and all extensor and flexor tendons were removed. To facilitate measurement of range of motion the middle finger was disarticulated at the metacarpophalangeal joint to allow a threaded Steinmann pin to be inserted into the third metacarpal and a second threaded Steinmann pin was inserted into the radial shaft along its longitudinal axis. The distal radioulnar joint and supporting soft tissues were left intact. A longitudinal dorsal capsulotomy was made and the joints were inspected for evidence of intracarpal ligament injury. Two specimens with scapholunate ligament injury were excluded, leaving 7 specimens for this study. The arthrotomy then was sutured closed for all measurements.
A cylindric jig was used to stabilize the cadaver to reproducibly record contact pressures and areas with the wrist held in the neutral position. The jig had 4 appropriately sized slots cut in it at 90° to each other. The specimen was held in the cylindric jig with the wrist in neutral position, and smooth Steinmann pinswere drilled through these precut slots in the jig through the shafts of the radius and the third metacarpal. These pins were left in the specimen throughout all surgical manipulations and measurements. In this way the specimen could be removed from and replaced back into the jig with the pins maintaining the wrist in neutral position while inside of the jig. These pins also prevented motion and translation of the wrist during loading of the carpus.
After the specimen had been prepared the shaft of its radius was placed in a clamp and motion was measured (eg, flexion, extension, ulnar deviation, and radial deviation). A pilot study had shown goniometric measurements to be reproducible consistently within 1° to 2°. Goniometric measurements were performed, aided by the threaded Steinmann pins preplaced in the intramedullary canals of the radius and third metacarpal. Similar to a previous study of fresh cadaveric specimens, gravity was the only force required to deviate the wrist and produce angular displacement in the plane of motion.4 No additional weights aside from the aforementioned Steinmann pins were used. The specimen was rotated as necessary to measure the appropriate direction of motion. Similar to a previous study4 the natural deviation from the major plane of motion (eg, radial deviation in extension, ulnar deviation in flexion, extension in radial deviation, and flexion in ulnar deviation) was not prohibited to measure the true 2-dimensional representation of the natural 3-dimensional motion of the wrist. Three trials were performed and the results were averaged for each measurement.
To measure contact pressures and areas the dorsal capsulotomy was opened and appropriately sized ultra low prescale pressure-sensitive film (Fuji; Sensor Product Inc., East Hanover, NJ) was inserted into the radiolunate joint. The film was kept dry while in the radiolunate articulation by using custom-made plastic covers. Any film that became wet was excluded and the trial was redone. The dorsal capsulotomy was repaired, with care taken to ensu
re the stability of the film in the radiolunate joint. The perpendicular pins through the radial shaft and third metacarpal then were placed into the precut slots in the jig to hold the specimen in an upright position with the wrist in neutral position. The pins also held the specimen away from the jig walls to avoid friction between the jig and the specimen. To load the wrist joint a predetermined 44 N load was applied to the third metacarpal through its perpendicular pins for 60 seconds. The weight was then removed, the capsulotomy was opened, and the film was removed. At least 4 separate trials were conducted and averaged for each specimen. Any evidence of translation of the film out of the radiolunate articulation or subluxation of the lunate in its fossa disqualified the trial.
Before starting the experiments the film was calibrated by applying known loads through a 1-cm cylinder. Room temperature and humidity were kept constant throughout the day. Each specimen had all measurements completed the same day they were started. All film was recorded and digitized within 3 hours to prevent eroding of the color patterns. The contact print was processed by a software program (Image software; Scion Inc., Frederick, MD). Preliminary studies were performed to verify the accuracy and resolution of the entire system.
The contact area was defined as the area with pressure higher than the threshold of the ultra low prescale pressure-sensitive film. The mean contact pressure was the average pressure of the contact area.
A 4-corner midcarpal fusion (lunate, triquetrum, capitate, hamate) was simulated by rigidly fixing the lunate, triquetrum, capitate, and hamate in situ with a spider plate (KMI, San Diego, CA) using a standard technique: the intersection of the 4 bones was reamed to inset the plate, which was countersunk 2 mm below the dorsal cortex. Two screws were placed into each bone. The scaphoid was retained without surgical manipulation. All measurements were repeated.
The scaphoid then was included in the simulated fusion by rigidly fixing it to the simulated 4-corner fusion mass with 2 cannulated screws (Acutrak; Acumed, Hillsboro, OR) using a standard technique. All measurements were repeated.
The screws then were removed and the scaphoid was excised. Care was taken to prevent injury to the extrinsic volar ligaments, specifically the radioscaphocapitate ligament. All measurements were repeated.
Statistics were performed by calculating the mean and SD in each group. Repeated measures analysis of variance with post hoc comparison of Tukey test was used to detect any difference in the range of motion, joint contact area, and pressure between the 4 groups: intact specimens, after 4-corner fusion with scaphoid retention, after 4-corner fusion with scaphoid inclusion, and after 4-corner fusion with scaphoid excision. All differences were considered significant at a probability level of 95% (p < .05).
Results
The range of motion for the intact specimen, after 4-corner fusion with scaphoid retention, scaphoid inclusion, and scaphoid excision are presented in Table 1 and Figure 1.
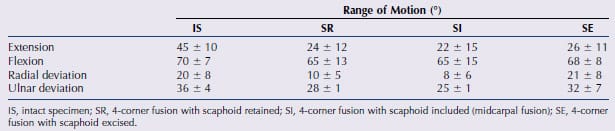
Table 1. Mean and SD for Range of Motion
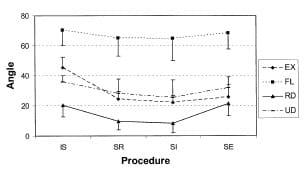
Figure 1. Range of motion after various procedures. IS, intact
specimen; SR, 4-corner fusion with scaphoid retained; SI,
4-corner fusion with scaphoid included (midcarpal fusion);
SE, 4-corner fusion with scaphoid excised. EX, extension; FL,
flexion; RD, radial deviation; UD, ulnar deviation.
There was a statistically significant difference in extension between the 4 groups (p = .0002). Compared with the intact specimen there was a significant decrease in extension after 4-corner fusion regardless of scaphoid retention (p < .01), scaphoid inclusion (p < .01), or scaphoid excision (p < .01). After 4-corner fusion there was no significant difference in extension between scaphoid retention, scaphoid inclusion, or scaphoid excision; there seemed to be a trend with scaphoid excision allowing greater extension than scaphoid inclusion or scaphoid retention, but this did not reach statistical significance.
Compared with the intact specimen there was no statistically significant difference in flexion after 4-corner fusion with scaphoid retention, scaphoid inclusion, or scaphoid excision (p = .24). After 4-corner fusion there seemed to be a trend with scaphoid excision allowing greater flexion than scaphoid inclusion or scaphoid retention, but this did not reach statistical significance.
There was a statistically significant difference in radial deviation between the 4 groups (p = .0004). Compared with the intact specimen there was a significant decrease in radial deviation after 4-corner fusion with either scaphoid retention (p < .05) or scaphoid inclusion (p < .01). After 4-corner fusion scaphoid excision led to a statistically significant increase in radial deviation compared with scaphoid retention (p < .01) or scaphoid inclusion (p < .01).
There was a statistically significant difference in ulnar deviation between the 4 groups (p = .003). Compared with the intact specimen there was a significant decrease in ulnar deviation after 4-corner fusion with either scaphoid retention (p < .05) or scaphoid inclusion (p < .01). After 4-corner fusion there was no significant difference in ulnar deviation between scaphoid retention, scaphoid inclusion, or scaphoid excision; there was a trend for scaphoid excision to allow greater ulnar deviation than scaphoid retention or scaphoid inclusion, but this did not reach statistical significance.
The radiolunate contact characteristics for the intact specimen and after 4-corner fusion with scaphoid retention, scaphoid inclusion, and scaphoid excision are presented in Table 2 and Figure 2.
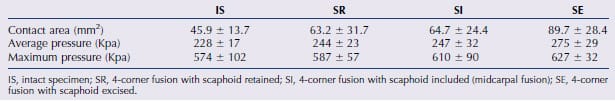
Table 2. Mean and SD for Contact Area, Mean, and Maximum Contact Pressure
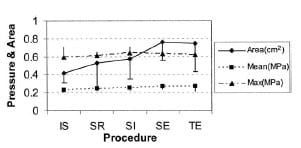
Figure 2. Average contact area, mean and maximum contact
pressure after various procedures. IS: intact specimen; SR:
4-corner fusion with scaphoid retained; SI: 4-corner fusion
with scaphoid included (midcarpal fusion); SE: 4-corner fusion
with scaphoid excised.
There was a statistically significant difference in radio
lunate contact area between the 4 groups (p = .0002). Compared with the intact specimen there was no significant difference in radiolunate contact area after 4-corner fusion with either scaphoid retention or scaphoid inclusion. After 4-corner fusion scaphoid excision led to a significant increase in radiolunate contact area compared with the intact specimen (p < .01) and specimens after 4-corner fusion with either scaphoid retention (p < .05) or scaphoid inclusion (p < .05).
There was a statistically significant difference in mean radiolunate contact pressure between the 4 groups (p = .005). Compared with the intact specimen there was no significant difference in mean radiolunate contact pressure after 4-corner fusion with either scaphoid retention or scaphoid inclusion. After 4-corner fusion scaphoid excision led to a significant increase in mean radiolunate contact pressure compared with the intact specimen (p < .01), but not compared with after 4-corner fusion with either scaphoid retention or scaphoid inclusion. There was no statistically significant difference in maximum radiolunate contact pressure between the intact specimen and after 4-corner fusion with either scaphoid retention, scaphoid inclusion, or scaphoid excision (p = .25).
Discussion
Compared with the intact specimen 4-corner fusion led to a significant decrease in extension, radial deviation, and ulnar deviation. After 4-corner fusion there was no significant difference in motion between scaphoid retention and scaphoid inclusion. After 4-corner fusion scaphoid excision allowed significantly greater radial deviation compared with scaphoid retention and scaphoid inclusion; there was a trend for scaphoid excision to allow greater extension, flexion, and ulnar deviation compared with scaphoid retention and scaphoid inclusion, but this did not reach statistical significance.
Compared with the intact specimen 4-corner fusion with scaphoid retention or scaphoid inclusion did not lead to a significant change in radiolunate contact characteristics. Similarly there was no statistically significant difference in mean or maximal contact pressures between 4-corner fusion with scaphoid retention or scaphoid excision. After 4-corner fusion scaphoid excision led to significantly greater radiolunate contact area compared with the intact specimen and 4-corner fusion with either scaphoid retention or scaphoid inclusion. After 4-corner fusion scaphoid excision also led to a significantly greater mean radiolunate contact pressure compared with the intact specimen but not compared with 4-corner fusion with scaphoid retention or scaphoid excision. None of the surgical manipulations had a significant effect on maximum radiolunate contact pressure.
At first glance it may seem unusual that with a constant applied force both area and pressure increased after 4-corner fusion with scaphoid excision. It must be remembered, however, that only the radiolunate articulation’s contact area and pressure were measured. With reference to the radiocarpal joint the applied load was distributed between the radiolunate and radioscaphoid articulations. After scaphoid excision, with the load on the wrist kept constant, all of the applied force now was transmitted through the radiolunate articulation. So although the force applied to the wrist was kept constant, the relative load experienced by the radiolunate joint increased, leading to an increase in both radiolunate contact area and pressure.
Although scaphoid excision led to a statistically significant increase in mean radiolunate pressures it is unclear whether this increased pressure is clinically important. Studies have shown that the radiolunate articulation holds up well after 4-corner fusion with scaphoid excision (the scaphoid lunate advanced collapse procedure) and that arthritis of the radiolunate articulation occurs rarely if at all.1–3,9 This may be because of the spheric nature of this articulation. As contact forces increase, the radiolunate contact area also increases, thus lowering contact pressures by uniformly distributing the increased load over an increased area, thereby decreasing the potential for cartilage overload. Although comparisons across studies are not possible, reports of midcarpal fusion including the scaphoid have shown a small percentage of patients with radiographic arthrosis at follow-up evaluation.10,11
When performing 4-corner arthrodesis for lunatotriquetral dissociation, midcarpal instability, or isolated midcarpal arthritis the surgeon has the option of scaphoid retention, scaphoid inclusion, or scaphoid excision. Compared with scaphoid retention and inclusion, scaphoid excision allows significantly increased radial deviation and tends to allow greater extension, flexion, and ulnar deviation, although this did not reach statistical significance. Lack of motion is a common clinical complaint after 4-corner fusion. To retain as much motion as possible a surgeon may choose to excise the scaphoid during after 4-corner arthrodesis. Alternatively in the absence of radioscaphoid arthritis, one may consider 4-corner fusion with scaphoid retention if the increases in radiolunate contact pressure are of concern.
Motion in our cadaveric model was somewhat greater than that found by Seradge et al.4 Seradge et al4 noted 40° of extension, 60° of flexion, 26° of ulnar deviation, and 6° of radial deviation for intact specimens; 23° of extension, 29° of flexion, 19° of ulnar deviation, and 0.4° of radial deviation after 4-corner fusion; and 26° of extension, 25° of flexion, 17° of ulnar deviation, and 1° of radial deviation after 4-corner fusion with scaphoid inclusion.4 They noted that the wrist maintained 50% of its flexion-extension arc and 40% of its ulnar deviation after 4-corner fusion with scaphoid inclusion, compared with 76% and 59% in this study. Gellman et al5 noted that the midcarpal joint was responsible for 46% of extension, 36% of flexion, 57% of ulnar deviation, and 55% of radial deviation. This is very similar to our findings for extension and radial deviation. In this study the cadavers lost less flexion (7%) and ulnar deviation (22%) after midcarpal fusion. Meyerdierks et al6 reported that simulated scapholunocapitate fusion caused a loss of 27% of the flexion-extension arc. This is similar to our findings of 23% loss of the flexion-extension motion arc after 4-corner fusion with either scaphoid retention or scaphoid inclusion. We noted a 32% loss of radioulnar deviation after 4-corner fusion.
This study used more rigid fixation than did previous models of simulated wrist fusions that relied on external fixation or intercarpal pins to stabilize the carpus.4-6 The spider plate and screws (Acutrak) represent modern rigid fixation systems. In this study 4-corner fusion led to a 47% decrease in wrist extension with only a 7% decrease in wrist flexion. This loss of wrist extension and relative preservation of flexion may have been owing to the in situ nature of the fusion, in contrast to the clinical situation in which it has been recommended that the surgeon reduce the lunate into slight flexion, and then volarly and ulnarly translate the capitate to maintain wrist extension without developing dorsal radiocarpal impingement.1,2 It is possible that although the arthrotomy was closed tightly before all measurements, the surgical manipulations may have weakened the dorsal soft-tissue constraints, therefore increasing flexion. This was a comparative study, however, in which each cadaveric wrist served as its own control. Therefore the relative effects of the various surgical manipulations still should be valid.
This study still had several limitations. Because of current difficulties in obtaining cadavers, only 7 w
ere used. Gellman et al5 used 12 cadavers, Meyerdierks et al6 used 11 cadavers, and Seradge et al4 used 10 cadavers. Although more cadavers allow a narrower SD and a greater power to determine significant differences in measured parameters, Viegas et al12,13 used only 5 cadavers in 2 biomechanical studies of the wrist, including one on intercarpal fusions. It is possible that with a greater number of specimens some of the noted trends might have reached statistical significance.
The usual limitations of the film (Fuji) were present. Color density can fade after a few hours of exposure to light. Therefore it has been recommended that the film be digitized within 8 hours of exposure.14 We digitized all film within 3 hours to try to minimize this artifact.
Ulnar variance was not controlled strictly. The ulna was cut 7 cm proximal to the distal radioulnar joint to allow us to clamp the radius circumferentially and so that we could measure all directions of wrist motion using gravity as the deforming force. The triangular fibrocartilage, distal radioulnar joint capsule, extensor carpi ulnaris subsheath, and enough interosseous membrane were left undisturbed, however, to avoid obvious distal radioulnar joint destabilization. The specimens always were placed in the jig in identical fashion, with no deforming forces on the ulna or the distal radioulnar joint. We noted no change in ulnar variance or distal radioulnar joint instability throughout specimen manipulations and testing. If any error was introduced by mild undetected changes in ulnar variance that caused the ulnocarpal joint to avoid bearing its appropriate load, it would be to overestimate the amount of increase in radiolunate contact pressures after scaphoid excision. Each specimen acted as its own control, however, and we believe that the relative changes in radiocarpal contact measurements were not influenced significantly by any changes in ulnar variance.
References
- Watson HK, Weinzweig J, Guidera PM, Zeppieri J, Ashmead D. One thousand intercarpal arthrodeses. J Hand Surg 1999;24B:307–315.
- Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and fourcorner arthrodesis. J Hand Surg 2001;26A:94–104.
- Tomaino MM, Miller RJ, Cole I, Burton RI. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg 1994;19A:134–142.
- Seradge H, Owens W, Seradge E. The effect of intercarpal joint motion on wrist motion: are there key joints? An in vitro study. Orthopedics 1995;18:727–732.
- Gellman H, Kauffman D, Lenihan M, Botte MJ, Sarmiento A. An in vitro analysis of wrist motion: the effect of limited intercarpal arthrodesis and the contributions of the radiocarpal and midcarpal joints. J Hand Surg 1988;13A:390–395.
- Meyerdierks EM, Mosher JF, Werner FW. Limited wrist arthrodesis: a laboratory study. J Hand Surg 1987;12A:526–529.
- Taleisnik J. Subtotal arthrodeses of the wrist joint. Clin Orthop 1984;187:81–88.
- Weiss LE, Taras JS, Sweet S, Osterman AL. Lunotriquetral injuries in athletes. Hand Clin 2000;16:433–438.
- Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg 1995;20A:965–970.
- Rotman MB, Manske PR, Pruitt DL, Szerzinski J. Scaphocapitolunate arthrodesis. J Hand Surg 1993;18A:26–33.
- Siegel JM, Ruby LK. Midcarpal arthrodesis. J Hand Surg 1996;21A:179–182.
- Viegas SF, Patterson RM, Peterson PD, Pogue DJ, Jenkins DK, Sweo TD, et al. Evaluation of the biomechanical efficacy of limited intercarpal fusions for the treatment of scapho-lunate dissociation. J Hand Surg 1990;15A:120–128.
- Viegas SF, Tencer AF, Cantrell J, Chang M, Clegg P, Hicks C, et al. Load transfer characteristics of the wrist. Part II. Perilunate instability. J Hand Surg 1987;12A:978–985.
- Patterson R, Pogue D, Viegas S. The effects of time and light exposure on contact and pressure measurements using Fuji prescale film. Iowa Orthop J 1997;17:64–69.
From the Department of Orthopaedic Surgery, Baylor College of Medicine; and the Houston Veteran’s Affairs Medical Center, Houston, TX.
Received for publication February 27, 2003; accepted in revised form July 8, 2003.
No benefits in any form have been received or will be received by a commercial party related directly or indirectly to the subject of this article.
Reprint requests: Jeffrey E. Budoff, MD, 6550 Fannin, #2525, Houston, TX 77030.
Copyright © 2003 by the American Society for Surgery of the Hand
0363-5023/03/28A06-0004$30.00/0
doi:10.1016/S0363-5023(03)00372-1


