Arthur Huang a, M.L. Hull a,b,*, Stephen M. Howell a,b
a Biomedical Engineering Program, Department of Mechanical Engineering, University of California, Davis, CA 95616, USA
b Department of Mechanical Engineering, University of California, Davis, CA 95616, USA
Abstract
This study addressed the question of whether the level of compressive load would affect the conclusions from statistical analyses aimed at determining how well a lateral meniscal autograft restores tibial contact (as indicated by the maximum contact pressure, mean pressure, and contact area) to that of the intact knee. If statistical analyses indicated that normal tibial contact was not restored with a higher, more physiologic load, then a secondary question was whether an autograft surgically implanted with bone plugs would improve tibial contact compared to that in a meniscectomized knee. Nine, fresh-frozen human cadaveric knees were subjected to a low, non-physiologic compressive load of 400 N and a higher, more physiologic compressive load of 1200 N under three conditions (lateral meniscus intact, lateral meniscus removed and reimplanted as an autograft, and lateral meniscus removed). Contact pressure on the lateral plateau was measured with pressure sensitive film at 0o, 15o, 30o, and 45 o of flexion. At 400 N, pvalues from statistical analyses indicated that both the maximum and mean pressures with the autograft were comparable to those of the intact knee (p≥0.685). However, at 1200 N, p-values from statistical analyses indicated that both the maximum and mean pressures with the autograft were significantly greater than those of the intact knee (p≤0.0001). Therefore studies designed to evaluate tibial contact pressure for a meniscal transplant should use a higher, more physiologic compressive load, because lower loads overestimate the transplant’s effectiveness. Although none of the contact variables was restored to normal when the compressive load was increased to 1200 N, all of the contact variables were more normal than those of the meniscectomized knee. Thus, lateral meniscal allografts implanted using bone plugs can significantly improve contact pressure relative to a meniscectomized knee at the time of implantation.
Keywords: Meniscus; Contact pressure; Compression; Autograft; Fixation
Introduction
At implantation the load-bearing function of a meniscal allograft is determined by the method of fixation [1,5] and can also be affected by differences in placement, size, shape, and material properties from the original meniscus. Different methods of fixation can best be studied by reimplanting the original meniscus as an autograft, thus eliminating these possibly confounding effects. Two studies have used an autograft to investigate different methods for fixing a meniscal transplant, but the findings were conflicting. One study reimplanted a lateral meniscus and showed that the maximum pressure was similar to the intact knee at a non-physiologic compressive load of 310 N [5]. The other study reimplanted a medial meniscus and showed that the maximum pressure was greater than in the intact knee at a more physiologic compressive load of 1000 N [1]. The cause of this conflicting finding could be related to the use of different compressive loads. The current study was addressed the question of whether the level of compressive load would affect the conclusions from statistical analyses aimed at determining how well a lateral meniscal autograft would restore tibial contact (as indicated by the maximum contact pressure, mean pressure, and contact area) to that of the intact knee.
Contact pressure might not be restored to normal at higher, more physiologic loads, but this does not necessarily mean that the surgical fixation method used to implant the autograft is ineffective. If the tibial contact pressure were to remain significantly better than that of the meniscectomized knee, then the fixation method might still be effective. If statistical analyses indicated that normal contact pressure was not restored with the higher, more physiologic load, then a secondary question was whether an autograft surgically fixed to the tibial plateau using bone plugs would improve contact pressure compared to that of the meniscectomized knee.
Methods
Nine human, fresh-frozen cadaveric knees were obtained from five females and four males (average age = 55 yrs; range 34–68 yrs). Anteroposterior and lateral radiographs of each knee were obtained to verify lack of joint space narrowing, osteophytes, chondrocalcinosis, and prior surgery.
Before testing, each knee was prepared for mechanical alignment in a load application system. Soft tissues within 10 cm of the joint line were left intact, and the rest were removed. To interface the specimen with the load application system, steel rods 12.5 mm in diameter were cemented into the femoral and tibial medullary canals and with PMMA.
Each knee was then aligned in a load application system [2]. The knee was aligned using a functional-axes approach, a technique with good repeatability [3]. After alignment, the specimen was potted using PMMA into hollow, rectangular tubes that allowed the specimen to be removed and returned to the testing apparatus while maintaining alignment.
The specimen was removed from the load application system, and a lateral femoral osteotomy was performed to facilitate the harvest and implantation of the lateral meniscus as an autograft. The osteotomy was modified from a previously described medial osteotomy [10]; the lateral condyle was removed rather than the medial condyle. A pilot study showed that the femur fractured at compressive loads above 800 N when the size of the detached portion of the lateral condyle was the same as described for medial exposure. Therefore we reduced the size of the detached condyle so that 1200 N could be applied without fracture.
Following the osteotomy, the lateral tibial plateau was used to create a template for the pressure sensitive film that was used to measure contact pressure on the tibial plateau. A 0.8 mm thick Teflon template of roughly the same size as the lateral meniscus was inserted under the meniscus and adjusted in form until it fit snugly upon the articular surface. The properly sized template was then used as a guide to cut packets of pressure sensitive film.
Both super-low and low range pressure film (Fuji Prescale Film; C Itoh, New York, NY) were used [11]. Super-low range film was used to measure pressures ranging from 0.5 to 2.5 MPa, because it provided a lower rated pressure threshold than the low range film, t
hus giving a more accurate measurement of contact area. Low range film was used to measure pressures ranging from 2.5 to 10 MPa, because previous studies have shown that super-low range film saturates under some joint conditions [1], thus underestimating the measurement of maximum pressure.
The pressure sensitive film was encapsulated in polyethylene packets to protect it from joint fluid and changes in humidity. The film packets were 0.25 mm thick, including the ‘‘A’’ dye layer and the ‘‘C’’ stain layer. All packets for a particular specimen were sealed simultaneously to control for humidity, which affects the stain properties of the film [9].
Following preparation of the film packets for each knee specimen, the specimen was preconditioned in the load application system. The system constrained flexion at a predetermined angle while applying compressive loads. Unconstrained motion was permitted in all other degrees of freedom [2]. The specimen was preconditioned by increasing the compression load to 1200 N over a 15-s interval, maintaining that load for 5 s, and then removing the load. Three complete loading cycles were applied at 0o and 45o of flexion.
The contact pressure of the intact knee was measured with the pressure sensitive film as compressive load was applied using the load application system. Three factors were controlled during the exposure of the pressure sensitive film: shear, overshoot, and loading time [10]. Three repetitions were made at each of the four randomized flexion angles of 0o, 15o, 30o, and 45o and at each of two randomized load levels of 400 and 1200 N, chosen to represent 1/2 body weight (BW) and 1 1/2 BW, respectively.
The specimen was then removed from the load application system to remove the lateral meniscus and harvest the autograft. A 2.4 mm diameter K-wire was drilled through the center of the posterior horn of the meniscus across the tibial metaphysis exiting distally on the anteromedial aspect of the tibia. A second K-wire was drilled through the center of the anterior horn, exiting distally on the posterolateral aspect. The meniscus was detached from the periphery leaving a 1–2 mm wide meniscal rim. A 10 mm cannulated reamer was then drilled from distal to proximal over each guide wire to within 15 mm of the tibial plateau. A cannulated coring reamer (10 mm outside diameter and 8 mm inside diameter; Acufex, Waltham, MA) was advanced within the tunnel up to the joint line to form bone plugs 8 mm in diameter and 15 mm in length attached to the horns of the meniscus. To prevent failure of the bone plugs during compressive loading of the joint, the plugs were reinforced with screws and PMMA [1].
The contact pressure was measured using the protocol for the intact knee with the autograft reimplanted and with the lateral meniscus removed (total meniscectomy). The autograft was secured to the plateau by cementing the bone plugs into the bone tunnels drilled when forming the autograft. The meniscectomy was performed by removing the autograft from the tibial plateau. The autograft was removed by removing the bone plugs. The preconditioning cycles were reapplied to the knee after each of the two surgical techniques was completed.
Calibration curves were used to convert the intensity of the film stain to a pressure value [6]. Because the film exposure is determined by both pressure and humidity, the relative humidity was recorded just before each specimen was tested. Calibration curves were generated for three different humidities (31%, 38%, and 42%) to encompass the range of relative humidities recorded. For each humidity, the super-low range film was calibrated from 0.25 to 4.0 MPa in 0.25 MPa increments; low range film was calibrated from 2.5 to 7.0 MPa in 0.25 MPa increments. The calibration loads were applied using a servohydraulic materials testing system (Model 858, MTS, Minneapolis, MN) and a previously described setup [9]. The exposed pressure stains were then transformed into color images using a high resolution scanner (Model 4c, Hewlett-Packard Corp, Palo Alto, CA). The color images were converted into 8-bit grayscale images, and the average grayscale value was measured using image analysis software (NIH Image, version 3b for Windows NT, Scion Corporation, Frederick, MD). Finally, a calibration curve relating pressure to grayscale value was derived using a fourth order polynomial regression [9].
Following testing of the cadaveric knees, all film packets exposed at a specific combination of joint condition and load level over the four flexion angles were scanned simultaneously for consistency [10]. From the calibrated images, three contact pressure variables were computed including the maximum pressure, contact area, and mean pressure. The maximum pressure (PMAX) was obtained from the low range of pressure film. The total contact area (A) was obtained from the super-low range of pressure film. The mean pressure (P) was obtained from both the super-low and low range pressure films. The contact area (AL) and mean pressure (PL) were determined for the low range film. From the super-low range film, the contact pressure for the area corresponding to that of the low range film was first set to zero. Then the mean pressure (PD) and the contact area (AD) of the remaining donut-shaped region of interest were calculated (Fig. 1). The mean pressure (P) for the composite image was calculated from
Average values for these contact pressure variables were calculated from the three repetitions at each combination of joint condition, flexion angle, and load level.
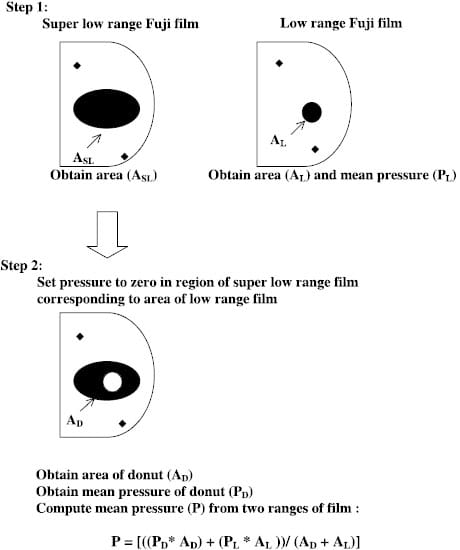
Fig. 1. – The technique used to calculate the mean pressure from two ranges of pressure sensitive film.
Statistical analyses
To determine how well the autograft restored contact pressure variables to normal and to determine whether the contact pressure variables for the autograft were better than those for the meniscectomized knee, two-factor analyses of variance (ANOVA) blocked by specimen were performed at each load level with the two factors being joint condition at three levels (intact knee, knee with the autograft, meniscectomized knee) and flexion angle at four levels. The response variables included maximum pressure, mean pressure, and contact area. Thus, a total of sixANOVAswere performed (two load levels x three dependent variables); the within-specimen interaction term joint condition x flexion angle) was suppressed in each. If significant differences were detected (p < 0:05) between joint conditions, then the different joint conditions were contrasted in pairs and a p-value was generated to indicate whether or not the paired joint conditions differed significantly.
The interaction term was suppressed based on results from a preliminary two-factor ANOVA that included the interaction term and that revealed five of the six interaction terms to be insignificant (p = 0.4457 at 400 N and 0.1409 at 1200 N for maximum pressure, p ¼ 0:0712 at 400 N and 0.0519 at 1200 N for mean pressure, p = 0.3950 at 400 N and 0.0256 at 1200 N for contact area). For the one interaction term that was significant, the interaction was not important because the additivity assumption still applied. Accordingly, the interaction term was suppressed in the above analyses, thus increasing the degrees of freedom in the error term and improving the ability to detect significant differences. All statistical analyses were performed with a commercially available software package (Version 8.2, SAS Institute Inc, Cary, NC).
Results
The level of compressive loading affected the conclusions from statistical analyses to determine whether the autograft restored both the maximum pressure and mean pressure to normal. At 400 N, the p-values from the ANOVAs were not significantly different for both the maximum (p = 0.685) and mean (p ≤ 0.956) pressures between the knee with the autograft and the intact knee (Table 1). At 1200 N however, the p-values indicated that both the maximum pressure and mean pressure with the autograft were significantly greater than that in the intact knee (p60:0001 for maximum, p = 0.016 for mean). Thus the autograft restored both the maximum pressure and mean pressure to normal with the 400 N load but not the 1200 N load. The conclusions from the statistical analyses changed because the difference in maximum pressure and mean pressure between the autograft and that of the intact knee increased with increasing load (Figs. 2 and 3).
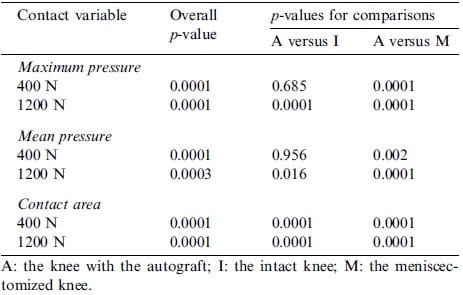
Table 1 – p-values from ANOVAs and the paired comparisons using the absolute values of the contact pressure variables
In contrast to the two pressure variables, the level of compressive loading did not affect whether the autograft restored the contact area to normal. At both 400 and 1200 N, the p-values indicated that the contact area with the autograft was significantly smaller (p≤0.0001) than that of the intact knee (Table 1). The conclusions from the statistical analyses did not change because the differences in contact area between the autograft and that of the intact knee were comparable at both the low and high load levels (Fig. 4).
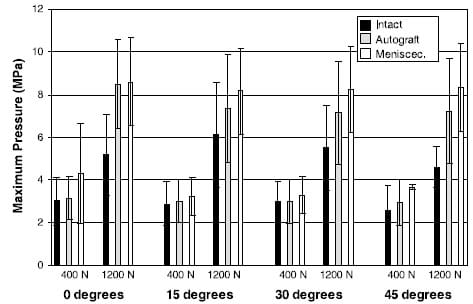
Fig. 2. – The average maximum pressure ( std dev) for the three joint conditions at each of the two compressive load levels and four flexion angles.
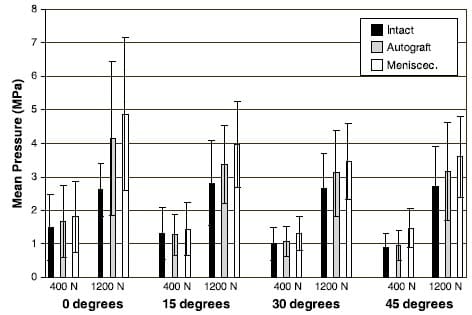
Fig. 3. The average mean pressure (±std dev) for the three joint conditions at each of the two compressive load levels and four flexion angles.
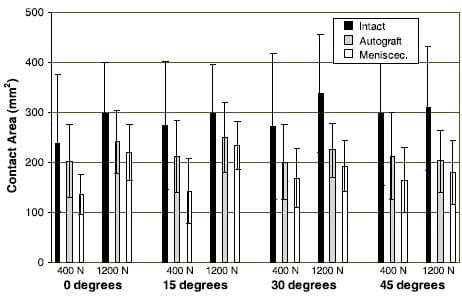
Fig. 4. The average contact area (±std dev) for the three joint conditions at each of the two compressive load levels and four flexion angles.
Although none of the contact variables were restored to normal when the compressive load was increased to 1200 N, all of the contact variables for the autograft were still better than those of the meniscectomized knee. The maximum pressure of the autograft was significantly lower (p≤0.0001), the mean pressure of the autograft was significantly lower (p ≤ 0.016), and the contact area of the autograft was significantly greater (p≤0.0001) than that of the meniscectomized knee (Table 1).
Discussion
Previous studies investigating tibial contact pressure using meniscal autografts reported conflicting findings regarding how well these tissues restored the maximum pressure to normal. Our findings were that: p-values from the statistical analyses indicated that both the maximum and mean pressures were comparable to normal with 400 N of compressive load but not with 1200 N; and fixing meniscal transplants using bone plugs did not restore contact pressure to normal at the time of implantation but did significantly improve contact pressure compared to that of the meniscectomized knee.
The most important finding was that the conclusions from the analyses to determine whether the autograft restored tibial contact pressure to normal depended on the level of compressive loading. Maximum and mean pressures in the knee implanted with an autograft were not different from normal with 400 N, but were significantly greater than normal with 1200 N. These results explain the conflicting reports between Chen et al. [5] and Alhalki et al. [1] on the effectiveness of meniscal autografts in restoring contact pressure in the intact knee. Testing the knee with the autograft at the higher, more physiologic load level accentuated the deficiencies in the surgical fixation method, when compared to testing at a lower load level.
The above finding occurred because both pressure quantities for the autograft were nearly identical to those for the intact knee when the load was limited to only 400 N (Figs. 2 and 3). Over all flexion angles the largest difference in maximum pressure was only 0.38 MPa, while the largest difference in mean pressure was only 0.17 MPa. However, with a 1200 N load, the largest differences in maximum and mean pressures became 3.28 and 1.53 MPa, respectively, indicating a non-linear relationship between the pressure difference from normal and the compressive load. Thus, pressure differences measured at lower loads cannot be scaled to higher loads. Consequently to correctly evaluate independent variables that may determine how well a meniscal allograft restores normal contact pressure on the tibial plateau, the compressive load level should be as close as possible to the physiologic load developed in walking. Independent variables include not only fixation methods, but also graft placement [14], geometry (size and shape of the graft) [15], and material properties [13].
The non-linear relationship between the pressure difference from normal and load level was confirmed in a post hoc three-factor repeated measures ANOVA where the interaction between joint condition and load level was of primary interest. The three factors were joint condition at three levels, compressive load at two levels, and flexion angle at four levels. From these analyses, the joint condition x load level interaction was significant for maximum pressure (p = 0.0005) and marginally insignificant for mean pressure (p = 0.069). The interaction for both pressure quantities would have been even stronger if the compressive load was greater than 1200 N because preliminary studies showed that the pressure difference between the autograft and the intact knee increased directly with increasing load for loads greater than 400 N.
Because the autograft eliminated the confounding effects of variability in geometric parameters, material properties, and location of attachment sites, our results might also be useful in determining whether surgical fixation methods are effective in restoring normal tibial contact pressure. Our method, however, differed from that used clinically. Cementing the bone plugs into the tibial tunnels was not analogous to surgical fixation in which bone plugs are held with sutures. Because of compliance in the sutures, the contact pressure may not be as close to normal as when bone plugs are cemented [1]. The clinical method also calls for suturing the peripheral rim of the transplant to the meniscal remnant, which was not done in the present study. This is not a limitation, however, because peripheral sutures do not affect contact pressure variables [1].
We can conclude that normal tibial contact pressure cannot be restored using bone plugs as the method of fixation at the time of implantation, similar to findings for the medial meniscus at a comparable level of compressive loading [1]. If compressive loading were to increase to 2 BW, thus approaching the load estimated during gait, then the differences from normal (Figs. 2 and 3) might be exacerbated.
One possible cause of the finding that the tibial contact pressure was not restored to normal for the autograft is the method of harvest from the intact knee. When the autograft was harvested, a portion of the rim of the meniscus remained attached to the retinaculum. When the autograft was implanted, the functional crosssectional area was reduced from that of the intact knee, hence reducing the tissue stiffness in the circumferential direction. Inasmuch as the circumferential tissue stiffness determines the tissue’s ability to support hoop stresses [13,15], a stiffness reduction could have allowed greater radial expansion with a concomitant increase in contact pressure.
Although the autograft when surgically implanted with bone plugs did not restore normal contact pressure, the contact variables for the autograft were better (pressures were lower and areas higher) than those for the meniscectomized condition at 1200 N for all flexion angles with one exception. Namely maximum pressure at 0o flexion was only 0.1 MPa less than that of the meniscectomized condition (Fig. 2). Although more detailed statistical comparisons of maximum pressure at individual flexion angles were not performed because the interaction was insignificant, but the similarity in maximum pressure at 0o flexion raises concern regarding the ability of a transplant to provide maximum pressure that is improved over that of the meniscectomized condition. However, during repetitive weight-bearing activities such as walking [12], stair climbing [12], and running [4], the knee remains flexed throughout the stance phase. Thus the similarity in the maximum pressures should not seriously compromise the transplant’s functionality.
Although our results showed that contact variables for the autograft implanted with bone plugs generally were better than those for the meniscectomized condition, which contact variables and what degree of improvement is necessary to prevent the development of osteoarthritis remain unknown. Presumably any improvement relative to the contact variables of the meniscectomized knee would retard degenerative changes. Accepting this assumption, lateral meniscal allografts implanted with bone plugs can still be justified as a surgical alternative to meniscectomy.
Limitations associated with using pressure sensitive film (method of inserting, exposing, and removing the film), with the use of elderly knee specimens, and with the load application system for measuring tibial plateau contact mechanics have been detailed previously [1,10], and are believed not to affect the conclusions from our study.
We assumed that performing the lateral osteotomy by exposing the lateral compartment of the knee did not affect the contact pressure of the lateral tibial plateau. This assumption was based on a previous study [10] that validated medial osteotomy as a benign procedure having no measurable effect (<1%) on the three contact pressure variables and on the two procedures being identical with the exception of the shallower cut in the lateral femoral condyle.
The osteotomy affected the level of compressive loading that could be applied to the knee without risk of fracturing the femur. Ideally, the applied compressive load should have been 1500 N (2 BW) to approximate the load across the knee during walking [7]. Pilot studies revealed that the osteotomy could not consistently support loads substantially greater than 1200 N (1 1/2 BW). If greater loads had been applied, then differences in both maximum and mean pressures between the autograft and intact knee would have been exacerbated, strengthening the interaction between the joint condition and load level. However, the 1200 N load developed a sufficiently strong interaction such that conclusions from the two-factor ANOVAs were different regarding the ability of the autograft to restore the maximum and mean pressure to normal.
During testing, the order in which the various joint conditions were tested could not be randomized thus presenting the possibility of carry-over effects. The intact knee had to be tested before the meniscus was harvested for the lateral autograft. The autograft was then reimplanted into the knee, and the contact pressure of the knee with the autograft was measured. Considering that the joint conditions could not be randomized in validating the osteotomy procedure [10] and that the procedure had no measurable effect on contact pressure, the lack of randomization should not have caused carry-over effects.
The maximum pressure determined from the low range film was influenced by the area over which it was computed. The image processing software determined maximum pressure as the maximum grayscale value corresponding to a single pixel. With an optical resolution of 300 dpi, the scanner provided a corresponding pixel area of 0.007 mm2, which yielded a spatial resolution greater than the 0.25 mm2 spatial resolution of the pressure film [8]. Accordingly, the pixel area did not filter any noise associated with the film and hence could have inflated the recorded maximum pressure. Moreover, the lack of filtering by the small pixel area could also have inflated the variability associated with the maximum pressure as the load increased to 1200 N (Fig. 2).
The area over which maximum pressure was computed did not affect our conclusions. To demonstrate this, the maximum pressure at one joint condition and flexion angle for each specimen was obtained by averaging pixel values within an area equal to the film resolution. Although the maximum pressure averaged over all specimens and the variability in the maximum pressure both decreased from the values in Fig. 2, the relative changes between the two load levels were preserved so that the results from the statistical comparisons remained the same.
In summary, we conclude that meniscal autografts and allografts implanted into cadaveric knees should be loaded as closely as possible to the compressive loading developed during walking to correctly evaluate the effect of independent variables on tibial contact pressure and that fixing meniscal transplants using bone plugs will not restore contact pressure to normal at the time of implantation in vivo but will significantly improve contact pressure compared to that of the meniscectomized knee.
Acknowledgements
The authors are grateful to the Whitaker Foundation for the financial support to undertake this project.
References
- Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med 1999;27:320–8.
- Bach JM, Hull ML. A new load application system for in vitro study of ligamentous injuries to the human knee joint. J Biomech Eng 1995;117:373–82.
- Berns GS, Hull ML, Patterson HA. Implementation of a five degree of freedom automated system to determine knee flexibility in vitro. J Biomech Eng 1990;112:392–400.
- Cavanagh PR. The biomechanics of lower extremity action during distance running. Foot Ankle 1987;7:197–217.
- Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 1996;12:174–81.
- Fuji Photo Film Company Ltd. Pressure Measuring Film. Fuji Prescale Film Instruction Manual, Tokyo, Japan, 1994.
- Komistek RD, Stiehl JB, Dennis DA, Paxson RD, Soutas-Little RW. Mathematical model of the lower extremity joint reaction forces using Kane’s method of dynamics. J Biomech 1998;31:185– 9.
- Liggins AB, Hardie WR, Finlay JB. The spatial and pressure resolution of Fuji pressure-sensitive film. Exp Mech 1995;35:166– 73.
- Liggins AB, Stanart JCE, Finlay JB, Rorabeck CH. Calibration and manipulation of data from Fuji pressure-sensitive film. In: Little EG, editor. Experimental mechanics: technology transfer between high tech engineering. New York: Elsevier; 1992. p. 61– 70.
- Martens TA. An in vitro osteotomy method to expose the medial compartment of the human knee. MS thesis in Biomedical Engineering. University of California at Dav
is, 1995. - Paletta Jr GA, Manning T, Snell E, Parker R, Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med 1997;25:692–8.
- Riener R, Rabuffetti M, Frigo C. Stair ascent and descent at different inclinations. Gait Posture 2002;15:32–44.
- Schreppers GJMA, Sauren AAHJ, Huson A. A numerical model of the load transmission in the tibio-femoral contact area. J Eng Med 1990;204:53–9.
- Sekaran V, Hull ML, Howell SM. Non-anatomic location of the posterior horn of a medial meniscal autograft adversely affects the pressure distribution on the tibial plateau at implantation in human cadaveric knees. Am J Sports Med 2002;30:74–82.
- Spilker RL, Donzelli PS. A biphasic finite element model of the meniscus for stress–strain analysis. In: Mow VC, Arnoczky SP, Jackson DW, editors. Knee meniscus; basic and clinical foundations. New York: Raven Press; 1992. p. 91–106.


