Michael Tanzer, MD; Christopher A. McLean, MEng; Eric Laxer, MD; John Casey, BEng; Abdul M. Ahmed, PhD
Objectives: To determine the effect of 5 different femoral components used in total knee arthroplasty (TKA) on the contact area and tracking characteristics of the nonresurfaced patella and to identify any design features that might adversely affect these characteristics. Design: An in-vitro study. Setting: The biomechanics laboratory, Department of Mechanical Engineering, McGill University, Montreal. Specimens: Six fresh-frozen cadaveric knee-joint specimens. Interventions: An unconstrained quadriceps simulator was used to apply the conditions of static lifting to the specimens first in their normal state and then sequentially implanted with femoral and tibial components of various designs (Miller/Galante II, Anatomic Modular Knee [AMK] System, Whiteside Ortholoc Modular, press-fit condylar and Insall–Burstein II). Outcome measures: Patellar 3-dimensional tracking characteristics, determined by using a 6 degrees-of-freedom electromechanical goniometer attached directly to the patella, and patellar contact pressure measurements, obtained using low-range Fuji Prescale film. Results: Articulation of the normal patella on a prosthetic femoral component resulted in alterations in the normal patellofemoral contact and tracking characteristics. The exact departure depended on the design of the prosthetic trochlea. Although all of the selected prostheses demonstrated satisfactory contact characteristics near extension, marked alterations occurred at higher flexion angles. With 90° or more of flexion, there was incompatibility between the geometries of the prosthetic notch of 2 femoral designs (AMK and PFC) and the normal knee. Conclusion: The design of the prosthetic femoral component must be taken into account when determining whether or not to resurface the patella at the time of TKA.
Early designs of prostheses used for total knee arthroplasty (TKA) did not allow for patellar resurfacing and were associated with a high rate of persistent patellofemoral pain postoperatively.1–6 As a result, modern prostheses have been designed to incorporate a resurfaced patella. Although patellar resurfacing decreased the frequency of patellofemoral pain, particularly in patients with rheumatoid arthritis, patellar complications have now become the second leading cause, after infection, for revision TKA.7 Patellar complications include maltracking, pain, loosening, wear, mechanical failure, softtissue impingement and patellar fracture.8–13
Early designs of prostheses used for total knee arthroplasty (TKA) did not allow for patellar resurfacing and were associated with a high rate of persistent patellofemoral pain postoperatively.1–6 As a result, modern prostheses have been designed to incorporate a resurfaced patella. Although patellar resurfacing decreased the frequency of patellofemoral pain, particularly in patients with rheumatoid arthritis, patellar complications have now become the second leading cause, after infection, for revision TKA.7 Patellar complications include maltracking, pain, loosening, wear, mechanical failure, softtissue impingement and patellar fracture.8–13
The alarming number of patellofemoral complications have influenced many orthopedic surgeons to selectively determine which knees require resurfacing or to abandon patellar resurfacing altogether at the time of TKA. Unfortunately, it is now apparent that up to 29% of patients with TKAs without patellar resurfacing may suffer anterior knee pain, 10% may require subsequent surgery for patellar resurfacing and one-third have difficulty climbing stairs.14–21 Picetti and colleagues19 evaluated 100 TKAs without patellar resurfacing at a mean of 4.5 years postoperatively: 29% of the knees continued to cause anterior knee pain. Barrack and associates15 found that at only 30 months’ follow-up,6 (10%) of the 60 knees that had not undergone patellar resurfacing required it subsequently because of anterior knee pain. In a study comparing 27 knees not subjected to patellar resurfacing with 100 knees with patellar resurfacing, Soudry and colleagues21 found that patients without a patellar button had more difficulty using the knee for stair climbing, and one-third avoided this activity altogether.
Because it is not apparent why some patients have patellofemoral symptoms after TKA without patellar resurfacing and others do not, the orthopedic surgeon cannot determine preoperatively with any certainty whether a patient will suffer patellofemoral symptoms after TKA without patellar resurfacing.
It has been speculated that anterior knee pain from a patella that is not resurfaced is secondary to altered patellofemoral biomechanics.16,20 The femoral components of current TKAs are designed to articulate with a corresponding patellar prosthesis. Articulation of the normal patella with the prosthetic femoral component poses a potential risk in terms of abnormal contact and tracking characteristics. The degree by which patellofemoral biomechanics will depart from normal depends on the design features of the femoral component. Therefore, we undertook a study to evaluate the effects of different femoral component designs on the contact and tracking characteristics of the unresurfaced patella and to identify any design features that may adversely affect these characteristics. Five designs were considered: Miller/Galante II (MG II) prosthesis (Zimmer, Warsaw, Ind.), Anatomic Modular Knee (AMK) System (DePuy, Warsaw, Ind.), Whiteside Ortholoc Modular (Ortholoc) prosthesis (Wright Medical Technology, Arlington, Tenn.), press-fit condylar (PFC) prosthesis (Johnson & Johnson, Warsaw, Ind.) and Insall– Burstein II (IB II) prosthesis (Zimmer). To allow direct comparisons of the effects of each design, corresponding to simulated loading conditions the foregoing characteristics were determined in knee joint cadaveric specimens first in their normal state and then sequentially implanted with the femoral and tibial components of each design.
Material and methods
Six fresh-frozen cadaveric knee joint specimens from 4 males and 2 females were used. The age of the donors ranged from 25 to 61 years (mean 38 years). To minimize prosthetic component inventory, only left knees with an anterior–posterior (A–P) femoral dimension of approximately 64 mm were selected. The specimens were verified to be free of abnormalities, patellar maltracking, arthritic changes and moderate to severe chondromalacia on visual and radiographic inspection. For mounting in the load simulator, the femurs and tibias were transected about 25 cm from the joint line and all skin, subcutaneous tissues and muscles removed. The knee capsule, ligaments and tendons were left intact, but a lateral retinacular release was done in all cases. No further patellar realignment procedures were carried out on any of the knees.
With respect to implantation of the prosthetic components in the frontal plane, the tibia and femur were cut perpendicular to their respective mechanical axes. In keeping with contemporary surgical practice, the femoral components were externally rotated by 3°. Although the thickness of the components varied from one design to another, we attempted in all cases to maintain the level of the joint line. With sequential prosthetic implantation, cuts were redone or custom-made shims inserted as required to maintain the original joint line and preserve softtissue balance. Restoration of the joint line was confirmed by postoperative radiographs. The femoral and tibial components were all placed centrally in the medial–lateral (M–L) direction. In the A–P direction, the tibial components were placed up to the posterior margin of the cut proximal tibia and aligned anatomically. A single posterior slope of 5° was adopted for the tibial cut, being the average slope recommended by the prosthetic component manufacturers. The specifications of the prosthetic components are listed in Table 1. In view of the fixed A–P dimension of the intact distal femurs selected, only a single size of each femoral component design was required, allowing direct comparisons of the contact area and tracking measurements among specimens without the need for scaling. With the exception of the Ortholoc prosthesis, the size of each femoral component design was such that its A–P dimension was the closest available to that of the intact femur while not exceeding it. However, only a large size was available for the Ortholoc prosthesis. Although its A–P dimension of 65 mm was sufficiently close to that of the intact femurs to retain it in our study, its accompanying M–L dimension of 79 mm (5 mm more than the next biggest femoral component) was excessive in 2 of the 6 specimens, resulting in collateral ligament impingement and flexion contracture. Therefore, in theses 2 cases, test measurements were not performed.
For the loading conditions, an unconstrained quadriceps simulator was used to apply the conditions of “static lifting,” an activity similar in nature to that of rising from a chair without the aid of an arm rest.22 In this simulation, a foot–floor reaction force of 334 N (half the body weight of a person weighing 68 kg) was applied to the tibia with its line of action being adjusted at each considered flexion angle in a manner commensurate with the activity. To counteract the flexional moment of the foot–floor reaction, 3 extensor muscle group forces — FL, FC and FM — were applied to the patella with their combined magnitude being correspondingly adjusted at each flexion angle. FL represented the effects of the vastus lateralis, FC represented those of the rectus femoris, the vastus intermedius and the vastus medialis longus and FM represented those of the vastus medialis oblique. The 3 forces were applied with steel cables through a brass cap fitted snugly on the outer surface of the patella. Their lines of action were based on previous work by Ahmed and associates.22 On the basis of muscle cross-sectional measurements in that report, the total extensor load was apportioned in a ratio of 1.75:2:1, respectively, for FL, FC, and FM. The flexion angles considered in the present study were 0°, 15°, 30°, 60°, 90° and 105°. Correspondingly over this flexion range, the total extensor load increased from about 90 N to 950 N.
Contact pressure measurements were taken with use of low-range Fuji Prescale film (Fuji Photo Film, Tokyo, Japan). The film sheets were enclosed in thin plastic packets (total thickness less than 0.3 mm) to protect them from the surrounding moisture and inserted superiorly between the patella and femur. To register the location of the contacting areas relative to the patella, landmarks were inscribed on each side of the patella in the mid-region and transcribed to each test-condition film packet using a dull point. Loading was gradually applied over 30 seconds and held for 60 seconds, followed by a quick unload. To determine the pressure distribution, the film was calibrated under the same load and unload conditions by exposing given areas of it to compressed air at given pressure levels against a flat ground surface. Both the test-condition and calibration traces were then digitized into gray level bitmaps (256 gray levels) using a flat-bed scanner (HP IC ScanJet; Hewlett Packard, Palo Alto, Calif.) and analyzed using an image analysis software program (Image Pro Plus; Media Cybernetics, Baltimore). The overall accuracy for the pressure and spatial measurements was ±0.05 MPa and ±0.1 mm respectively. The threshold and saturation levels of the film were approximately 1 MPa and 5.5 MPa respectively.
Results
The patellar 3-dimensional tracking characteristics were measured using a 6 degrees-of-freedom electromechanical goniometer attached directly to the patella. The tracking characteristics were described as 3 Euler rotations — flexion, tilt and spin — and 3 Cartesian translations — medial–lateral, anterior–posterior and proximal–distal. The rotation axes were based on the patella’s anatomically defined axes, whereas the translation axes were based on the anatomical axis of the femur and a line parallel to the posterior condyles. The initial position from which the displacements were measured in each specimen corresponded to that of the patella in the intact case at 15° of knee flexion. The overall accuracies for the rotations and translations were determined to be ±0.5° and ±0.5 mm respectively.
Statistical comparisons, between the cadaveric specimens in their normal state and sequentially implanted with the femoral and tibial components of each design, were carried out using a repeated one-way analysis of variance at each flexion angle for the following parameters: total contact area, percentage of the total contact area subjected to high pressures (more than 5 MPa) and patellar tracking. The Student–Newman–Keuls test was then used to further evaluate differences among the individual implant designs. A p value of less than 0.05 was considered significant.
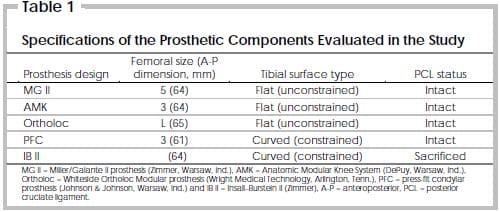
Table 1 – Specifications of the Prosthetic Components Evaluated in the Study
However, in deep knee flexion (90° and 105°), there was a pronounced decrease in the patellar contact area in the implanted cases (Table 2). The average contact area was 69% and 65% of the normal knee at 90° and 105° of knee flexion respectively (p = 0.002 at 90°, p = 0.004 at 105°). All of the 5 implants tested had significantly less patellar contact area than the normal knee at these higher flexion angles (p < 0.05). Furthermore, the implanted knees tended to demonstrate severely altered patellar contact distributions at 90° and 105° of knee flexion. Unlike the normal knee, in which the region of contact was characterized as a transverse band in deep knee flexion, the implanted specimens tended to have discrete isolated zones of contact on each facet (Fig. 1).
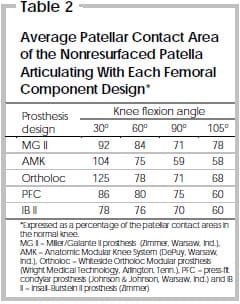
Table 2 – Average Patellar Contact Area of the Nonresurfaced Patella Articulating With Each Femoral Component Design
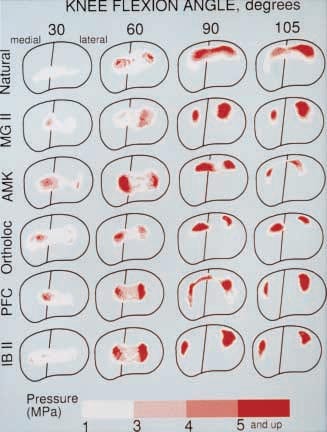
FIG. 1. Comparison of the contact pressure distributions measured in the intact articulation (first row) with those measured when the intact patella articulates with the femoral components of 5 different component designs used in total knee arthroplasty, for 4 different flexion angles (30°, 60°, 90° and 105°). MG II = Miller/Galante II prosthesis (Zimmer, Warsaw, Ind.), AMK = Anatomic Modular Knee prosthesis (DePuy, Warsaw, Ind.), Ortholoc = Whiteside Ortholoc Modular prosthesis (Wright Medical Technology, Arlington, Tenn.), PFC = press-fit condylar prosthesis (Johnson & Johnson, Warsaw, Ind.) and IB II = Insall–Burstein II prosthesis (Zimmer).
Patellar contact pressures varied depending on the implant used and the degree of knee flexion (Table 3). At 0 to 30°, most of the patellar contact area was associated with low contact pressures. Only 0.3% of the contact area in the normal knees and 0.3% to 5.0% of the contact area in the implanted knees demonstrated patellar contact pressures greater than 5 MPa at 30° of knee flexion (p = 0.2). Furthermore, there were no significant differences among any of the various implants. At 60° of flexion, articulation of the unresurfaced patella with the AMK, IB II, PFC and Ortholoc femoral components resulted in a significantly greater proportion of the patellar contact area being subjected to pressures greater than 5 MPa than when articulating with the normal knee (p < 0.05). Although increased patellar contact pressures occurred with 90° and 105° of flexion, this effect was most pronounced in the implanted cases. At 90° of flexion all implants had significantly greater proportions of their patellar contact areas subjected to pressures greater than 5 MPa compared with normal knees (p < 0.05). At 105° of flexion, the IB II, MG II and PFC prostheses continued to have a greater proportion of their contact areas subjected to these high pressures than normal knees (p < 0.05).
Incompatibility between the geometries of the AMK and PFC femoral intercondylar notches and the normal patella occurred at 90° and 105° of flexion. At these high flexion angles, the apex of the central ridge of the retropatellar surface impinged on the prosthetic intercondylar notch. The impingement either created a marked indentation into the apex of the patellar central ridge or resulted in frank displacement of the patella into the notch. This effect is illustrated in Fig. 1 where the pressure distributions are seen to undergo abrupt changes, outlining the shape of the notches. As a result of the patellar groove’s quick transition into the notch and its sharp border, indentation of the retropatellar surface was particularly severe with the AMK design.
In-plane tracking characteristics did not differ between the implanted specimens and the normal knees. There was no significant difference in patellar flexion, proximal–distal translation and A–P translation among any of the implanted knees, or between the implanted knees and the normal knees.
The out-of-plane tracking characteristics were altered to varying degrees when the normal patella was required to articulate with a prosthetic femoral prosthesis. From 15° to 30° of knee flexion, significant lateral tracking of the patella occurred at 15° with the MG II prosthesis (p < 0.05) and at 30° with the AMK, MG II and PFC prostheses (p < 0.05). On average, implantation of these prostheses resulted in patellar translations that were approximately 3 to 5 mm more lateral than that seen in the normal knee (p < 0.001). This lateral translation appeared to occur as a result of an intentional design feature of the femoral components to reduce maltracking and was not associated with clinically obvious patellar subluxation. From 60° to 105° of flexion, the implanted specimens demonstrated M–L patellar translation similar to that of the normal knee. Patellar spin similar to that in the normal knee was seen in all implants between 30° and 105° of knee flexion. Only from 0 to 15°, did patellar spin vary significantly among the normal knee and the IB II, PFC and Ortholoc prostheses (p < 0.05). Various implants demonstrated aberrant patellar tilt. Compared with the normal knee, increased medial tilt of the patella occurred with the Ortholoc prosthesis from 15° to 105° of flexion (p < 0.05), with the IB II prosthesis from 60° to 105° (p < 0.05) and with the PFC prosthesis at 90° and 105°.
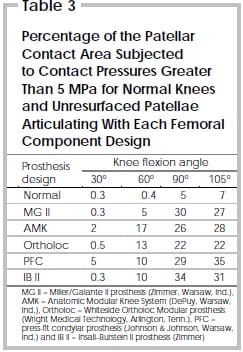
Table 3 – Percentage of the Patellar Contact Area Subjected to Contact Pressures Greater Than 5 MPa for Normal Knees and Unresurfaced Patellae Articulating With Each Femoral Component Design
Discussion
Alterations in normal patellofemoral contact and tracking characteristics can be expected when the unresurfaced patella is brought to articulate with a prosthetic femoral component. The exact departures will depend on the design of the prosthetic trochlea. At low flexion angles, patellar contact area, location and pressures were similar between implanted specimens and normal knees. However, with increasing flexion there was a profound alteration in patellar contact distribution, a progressive decrease in the patellar contact area and, as a result, a significant increase in patellofemoral contact pressures. At 90° and 105° of knee flexion, the implanted specimens tended to have only discrete isolated zones of contact on each facet of the patella, and these areas were subjected to higher than normal pressures. These findings may help explain why patients can experience difficulties carrying out activities that require loading the patellofemoral joint at high degrees of knee flexion, such as stair climbing. 21 Even patients who can ascend stairs normally when tested, may not do so in everyday life. Levitsky and associates18 found that although 53 (80%) of their 66 patients whose patella was not resurfaced were able to ascend stairs reciprocally when tested postoperatively in the office, only 24% climbed stairs reciprocally in their routine day-to-day activities.
At 90° and 105° of knee flexion, articulation of the unresurfaced patella with 2 of the femoral component designs resulted in impingement of the patella on the intercondylar notch. At these high flexion angles, the intercondylar notch design of both the AMK and PFC implants did not adequately support the patella, thereby allowing it either to be indented by or actually to displace into the notch. This lack of patellar support was due to the high, wide design of these prosthetic intercondylar notches. Yoshii and colleagues23 have noted the same findings in a cadaveric study of TKA with patellar resurfacing. Displacement of the patellar component into the intercondylar notch was avoided when the symmetrical femoral component being studied was modified so that its intercondylar notch was narrowed and shortened. This lengthened the patellar groove and maintained patellar support beyond 90° of flexion. It appears that femoral components with short patellar grooves and wide notches should be avoided if TKA is being contemplated without patellar resurfacing.
Previous attempts to identify risk factors that could predict which patients would develop patellofemoral pain after TKA without patellar resurfacing have been generally unsuccessful and even contradictory. Based on their study of 100 patients, Picetti and colleagues19 have recommended patellar resurfacing for all patients suffering from rheumatoid arthritis and for patients who have osteoarthritis if they complain of patellofemoral pain preoperatively, are more than 160 cm tall, weigh more than 60 kg and have advanced changes in the patella at the time of operation. In a prospective, randomized study of 118 knees, specifically addressing patellar resurfacing, Barrack and associates15 found no relationship between preoperative anterior knee pain, obesity or the grade of patellar chondromalacia and postoperative clinical outcome. Levitsky and associates18 proposed that in the absence of inflammatory or crystalline disease, younger and more active patients with a normal-shaped patella, normal tracking and articular cartilage do not require patellar resurfacing. Although various studies have recommended that patellar resurfacing be done routinely on all patients having rheumatoid arthritis, 15,18,19 others have suggested that rheumatoid arthritis is not a contraindication to nonresurfacing the patella.16,17,20,21,24 In these studies the authors, with the exception of Boyd and associates,16 have failed to take into account the possibility that the femoral prosthetic design may have a significant influence on the outcome of patients who did not undergo patellar resurfacing. It appears from our study that the differences in conclusions among the various studies with respect to risk factors and the results after TKA with and without patellar resurfacing, may be due to variations in the designs of the femoral component that subsequently affect patellar biomechanics. Therefore, conclusions from other studies may only be true for the specific implant evaluated. The etiology of patellofemoral pain after TKA in the patella that has not been resurfaced is probably multifactorial. However, the current study demonstrates that prosthetic design can adversely affect patellar biomechanics and should be considered a risk factor when deciding whether or not patellar resurfacing is required. This concept has been recognized by Boyd and associates16 who recommended routine resurfacing with TKA using the Duopatellar prosthesis (Johnson & Johnson). They implicated the symmetrical, nonconstrained patellofemoral joint as a factor in poor functioning of the patella. Similarly, Keblish and associates25 have indicated that prosthetic design will alter patellar function. They obtained excellent clinical and radiographic results following TKA with the low contact stress prosthesis (LCS; DePuy) without patellar resurfacing and have attributed it to the near anatomical shape of the femoral component.
To avoid subjecting the retropatellar surface of the unresurfaced patella to adverse contact conditions after TKA, the maximum contact stresses must not exceed their normal values. This is particularly important at high degrees of knee flexion, where the normal knee is subjected to high forces and patellofemoral symptoms are more common. In the current prosthetic designs for TKA evaluated in this study, this condition did not appear to be met. Whether recent TKA designs, which provide a deeper and more anatomic patellofemoral groove will allow normal patellofemoral kinematics and lower contact pressures remains unknown. Future designs should attempt to take into account the geometry of the normal patella if they are to be prescribed in TKA without patellar resurfacing. Alternatively, specific components should be designed solely to articulate with a patella that has not been resurfaced. The patellar surface of this component should conform to the normal trochlear topography and the intercondylar notch should be located and shaped so as to ensure smooth sliding of the unresurfaced patella at high flexion angles.
References
- Clayton ML, Thirupathi R. Patella complications after total condylar arthroplasty. Clin Orthop 1982;170:152-5.
- Insall JN, Ranawat CS, Agletti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg [Am] 1976;58(6):754-65.
- Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg [Am] 1979;61(2):173-80.
- Mochizuki RM, Schurman DJ. Patella complications following total knee arthroplasty. J Bone Joint Surg [Am] 1979;61 (6A):879-83.
- Murray DG, Webster DA. The variableaxis knee prosthesis. Two-year follow-up study. J Bone Joint Surg [Am] 1981;63 (5):687-94.
- Rananwat CS. The patellofemoral joint in total condylar knee arthroplasty. Pros and cons based on five- to ten-year follow-up observations. Clin Orthop 1986;205:83-9.
- Rand JA. Patellar resurfacing in total knee arthroplasty. Clin Orthop 1990;260:110-7.
- Aglietti P, Buzzi R, Gaudenzi A.
Patellofemoral functional results and complications with the posterior stabilized total condylar knee prosthesis. J Arthroplasty 1988;3:17-23. - Goldberg VM, Figgie HE, Inglis AE, Figgie MP, Sobel M, Kelly M, et al. Patellar fracture type and prognosis in condylar total knee arthroplasty. Clin Orthop 1988; 236:115-22.
- Grace JN, Rand JA. Patellar instability after total knee arthroplasty. Clin Orthop 1988;237:184-9.
- Lombardi AV, Engh GA, Volz RG, Albrigo JL, Brainard BJ. Fracture/dislocation of the polyethylene in metal-backed patellar components in total knee arthroplasty. J Bone Joint Surg [Am] 1988;70: 675-9 .
- Rosenberg AG, Andriachi TP, Galante JO. Patellar component failure in cementless total knee arthroplasty. Clin Orthop 1988;236:106-14.
- Stulberg SD, Stulberg BN, Hamati Y, Tsao A. Failure mechanisms of metalbacked patellar components. Clin Orthop 1988;236:88-105.
- Abraham W, Buchanan JR, Daubert H, Greer RB, Keefer J. Should the patella be resurfaced in total knee arthroplasty? Efficacy of patellar resurfacing. Clin Orthop 1988;236:128-34.
- Barrack RL, Wolfe MW, Waldman DA, Milicic M, Bertot AJ, Myers L. Resurfacing of the patella in total knee arthroplasty. A prospective, randomized, double-blind study. J Bone Joint Surg [Am] 1997;79:1121-31.
- Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg [Am] 1993;75:674-81.
- Enis JE, Gardner R, Robledo MA, Latta L, Smith R. Comparison of patellar resurfacing versus nonresurfacing in bilateral total knee arthroplasty. Clin Orthop 1990;260:38-42.
- Levitsky KA, Harris WJ, McManus J, Scott RD. Total knee arthroplasty without patellar resurfacing. Clinical outcomes and long-term follow-up evaluation. Clin Orthop 1993;286:116-21.
- Picetti GD, McGann WA, Welch RB. The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Joint Surg [Am] 1990;72:1379-82.
- Smith SR, Stuart P, Pinder IM. Nonresurfaced patella in total knee arthroplasty. J Arthroplasty 1989;4 Suppl:S81-6.
- Soudry M, Mestriner LA, Binazzi R, Insall JN. Total knee arthroplasty without patellar resurfacing. Clin Orthop 1986;205: 166-70.
- Ahmed AM, Burke DL, Yu A. In-vitro measurement of static pressure distribution in synovial joints — Part II: retropatellar surface. J Biomech Eng 1983;105: 226-36.
- Yoshii I, Whiteside LA, Anouchi YS. The effect of patellar button placement and femoral design on patellar tracking in total knee arthroplasty. Clin Orthop 1992;275: 211-9.
- Shoji H, Yoshino S, Kajino A. Patellar replacement in bilateral total knee arthroplasty. A study of patients who had rheumatoid arthritis and no gross deformity of the patella. J Bone Joint Surg [Am] 1989;72:853-6.
- Keblish PA, Varma AK, Greenwald S. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg [Br] 1994;76:930-7.


