Lars Carlson1,2, Bj õrn Albrektsson1,3 and Michael A. R. Freeman‘‘
The compression forces on the medial cortex of the femoral neck were measured in 6 cadaver specimens using pressure-sensitive film. A hip prosthesis was loaded in an Instron machine comparing the situation with retained versus resected neck. The results indicate that retaining the neck can be mechanically valuable
after total hip replacement have been identified, among which one of the most common is downward translational migration and varus rotational tilting of the component. Retentiqn of the neck should theoretically improve load transmission between the prosthesis and the femur. In cadavers, we compared the compression forces on the medial cortex when the neck was retained versus resected.
Material and methods
Six fresh proximal femoral specimens obtained at routine autopsy were stored at -20″ C, thawed, and prepared to accept the Freeman hip prosthesis using the same technique as that employed during surgery (Carlsson et al. 1987). The prosthesis has three neck lengths and three stem diameters: in each of the specimens the femur was reamed to 14 mm and a medium neck prosthesis with a 14-mm-diameter stem was inserted. As a consequence the varus lever arm was of the same length in all the tested specimens. The cortical support of the stem might have differed between different specimens; but because a comparison was always made between resected and retained necks in the same specimen, this difference in fit was neglected.
The distal end of the cadaveric femur was gripped in a cylindric holder in such a way that the shaft of the femur was vertical. Load was applied through the greater trochanter and via the prosthetic femoral head to simulate one leg stance. The system (Tanner et al. 1986) consisted of a 200-mm U-shaped channel, at one end attached to the greater trochanter via braided steel wire (Figure 2). A mavable plastic cup on the U-channel was mounted on the prosthetic head and load was applied on the medial end of the U using an Instron testing machine for strength of materials. Because of the leverages generated with this arrangement, the load applied through the Instron was mutiplied by approximately a factor of 3 on the femoral head.
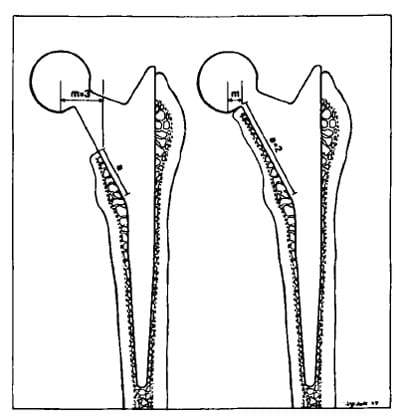
Figure 1. Illustration of the Freeman hip prosthesis with neck resected and neck retained. The moment arm acting to turn the prosthesis into varus in response to the vertical component of the resultant acting on the femoral head is approximately one third of that acting when the neck was resected. Similarly, the length of the medial neck cortex available to support the vertical load is approximately doubled by neck retention.
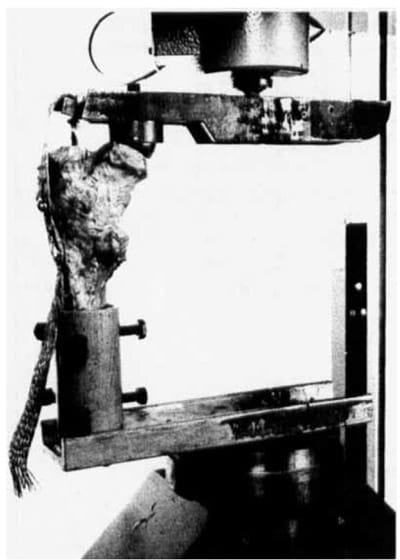
Figure 2. The experimental preparation with which load was applied to the femur in the laboratory.
The load applied to the medial cortex of the femoral neck was recorded by placing a piece of pressure-sensitive film between the medial edge of the prosthetic neck and the inner aspect of the femoral neck cortex. The film used was Fuji prescale film in three grades of sensitivity: 1) Super-Low Pressure (Specimen 6 only); 2) Low Pressure, sensitivity range 2-7 MPa; and 3) Medium pressure, range 7-25 MPa.
Because the inner surface of the medial neck cortex is not perfectly flat and because on the small scale it was composed of the stumps of a number of cut trabeculae, the staining pattern of the pressure-sensitive film was spotty rather than continuous. The color density varied from place to place within the sensitized area, and it proved impossible to measure accurately the area represented by each color. It was therefore not possible to obtain an accurate estimate of the magnitude of the total load applied to the bone in each case. We therefore made two measurements on each film as follows: 1) The total stained area on the film (i.e., the area where pressure was greater than the minimum sensitivity of the film); 2) The stained area expressed as a percentage of the total area (not the projected area) being studied.
For each test run a load of 800 N was first applied to the U-channel in order to “bed-down’’ the prosthesis. The load was then removed, the prosthesis extracted, and the film applied to the prosthesis. The prosthesis was reinserted and the U-channel was loaded for 2 minutes with 500 N. The load was reduced to zero, the femoral prosthesis removed, and the film retrieved for examination. Another piece of film was applied and the sequence repeated, but on this occasion raising the load to 800 N. In this way, loads of 1,500 and 2,400 N were applied to the femoral head. The femoral neck was then resected 15 mm proximal to the less trochanter and the loading sequence repeated.
Results
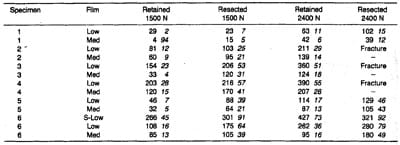
Table 1. Compression forces on the medial cortex of the femoral neck measured by pressure-sensitive film. Figures are total stained area (mm2) on the film and percentage of the total area studied
Specimens (Table 1) Nos. 2, 3, and 4 sustained a load of 2,400 N when the neck was retained. but fractured at a load of approximately 2,100 N after the neck had been resected. The fracture assumed the form of a vertical split extending downwards from the medial cortex of the transected femoral neck. The area stained was less when the neck was retained except in specimen 1. The percentage of the examined area that appeared to be carrying sufficient load to sensitize the Fuji film was less with the neck retained than when the neck was resected in all the specimens. These findings indicate that the average contact stress on the base of the medial neck was reduced by neck retention.
Specimens 1, 2, and 5 appeared to carry less load on the medial neck cortex than the remainder. These specimens all had narrow medullary canals and thus provided a tight press-fit for the femoral stem so that a higher proportion of load may have been carried through the stem than in the other specimens.
Discussion
Our study confirms and adds to the theoretic expectation summarized in Figure 1. showing that in the cadaver, resection of the neck results in an increase of the stresses on the remaining stump. The increased stress on the medial cortex of the neck is due mainly to three factors: First, the obvious decrease in the ar
ea of bone carrying load when the neck is resected; secondly, the longer moment arm tilting the prosthesis into varus; thirdly, a two-dimensional finite element model of a V-shaped wedge loaded into a funnel of matching shape shows the load to be distributed over the whole length of both sides of the V. If one side of the funnel is shortened, no load is borne on the remaining side above the level of the top of the shortened side: this load is transferred into the remaining part of the V (personal communication, Dr. A. L. Yettram, Brunel University, Uxbridge, Middlesex, England). According to this, when the neck is resected the greater trochanter may be stress-relieved above the level of neck resection, the additional load being applied to the remaining medial neck cortex and to the lateral cancellous bone at this level.
Because the resected neck was examined after the specimen had been loaded with the neck retained (there is no other way of doing the experiment), the objection could be raised that there might have been a less perfect canal pressfit in the neck-resected situation and thus transference of more load to the medial cortex of the neck. But because,the stem is tapered, repeated loading sequences would have the effect of tightening the stem.
The femoral neck has been retained during total hip arthroplasty for the past 5 years at the London Hospital, with encouraging preliminary results (Albrektsson et al. 1987). The arguments for retaining the neck and the counter arguments have been reviewed elsewhere (Freeman 1986).
Acknowledgements
References
- Albrektsson B E J, Freeman M A R, Carlsson L V, Tuke M A, Clark J M. Retention of the femoral neck: a method to enhance prosthetic fixation. J Orthop Surg Tech 1987:3;(2):99-124.
- Freeman M A. Why resect the neck? J Bone Joint Surg (Br) 1986;68(3) :346-9,
- Tanner E, Rasmussen G L, Bonfield W, Freeman M A R, Reed P E. A system for the modelling of the forces on the hip joint in one-legged stance. J Biomed Eng 1986; submitted.


